This Environmental Health & Safety guideline documentation is intended for researchers and laboratory personnel.
General Description
The purpose of this Guidance Document for Disinfectants and Sterilization Methods is to assist lab personnel in their decisions involving the judicious selection and proper use of specific disinfectants and sterilization methods.
IntroductionThe purpose of this Guidance Document for Disinfectants and Sterilization Methods is to assist lab personnel in their decisions involving the judicious selection and proper use of specific disinfectants and sterilization methods. For information concerning the proper disposal of all disinfected or sterilized waste, please refer to the Generators’ Guide to Hazardous Material / Waste Management.
Definitions
Antisepsis
A process involving the destruction or inhibition of mico-organisms in living tissue thereby limiting or preventing the harmful effects of infection.
Antiseptic
Typically an antiseptic is a chemical agent that is applied to living tissue to kill microbes. Note that not all disinfectants are antiseptics because an antiseptic additionally must not be so harsh that it damages living tissue. Antiseptics are less toxic than disinfectants used on inanimate objects. Due to the lower toxicity, antiseptics can be less active in the destruction of normal and any pathogenic flora present.
Autoclave
An autoclave is a high pressure device used to allow the application of moist heat above the normal-atmosphere boiling point of water.
Biocidal
Active substances and preparations which serve to repel, render harmless or destroy chemically or biologically harmful organisms.
Biocide
Substance or chemical that kills biological organisms.
Decontamination
The killing of organisms or removal of contamination after use, with no quantitative implication, generally referring to procedures for making items safe before disposal.
Disinfectant
A germicide that inactivates virtually all recognized pathogenic microorganisms but not necessarily all microbial forms. They may not be effective against bacterial spores.
Disinfection
A procedure of treatment that eliminates many or all pathogenic microorganisms with the exception of bacterial spores.
Germicide
An agent that destroys microorganisms, particularly pathogenic microorganisms.
Pathogenic
A microbe or other organism that causes disease.
Sanitization
The process of reducing microbial contamination to an acceptable “safe” level. The process of cleaning objects without necessarily going through sterilization.
Steam Sterilization
Autoclave, the process of sterilization by the use of heated steam under pressure to kill vegetative microorganisms and directly exposed spores. Common temperature and pressure for being effective is 121°C (250°F) at 15 psi (pounds per square inch) over pressure for 15 minutes. Special cases may require a variation of the steam temperature and pressure used.
Sterilization
The complete elimination or destruction of all forms of life by a chemical or physical means. This is an absolute not a relative term.
Disinfectants
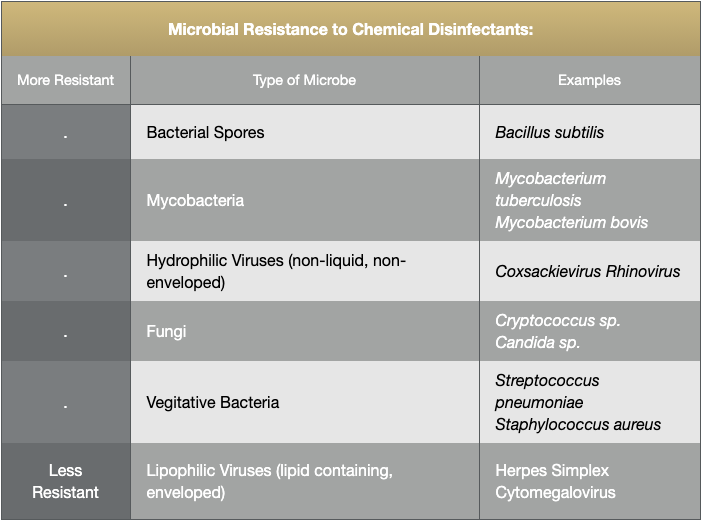
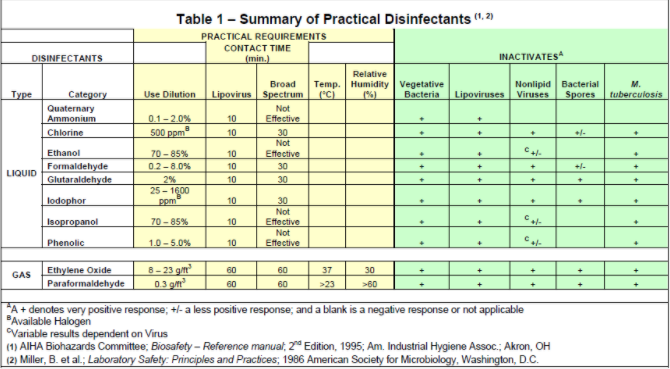
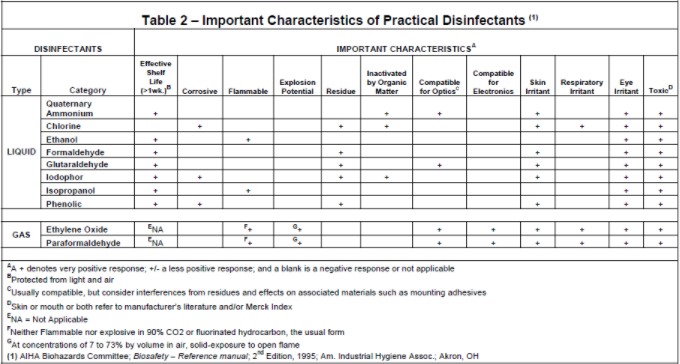
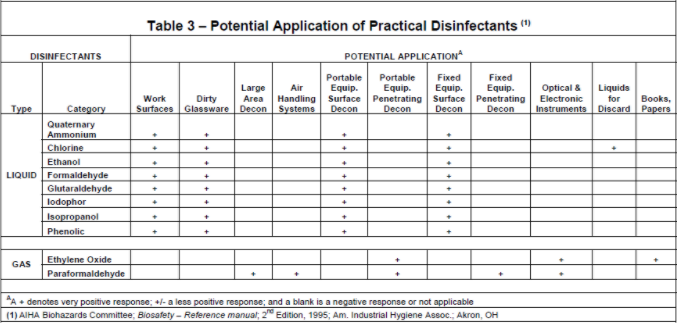
The information presented in this section will provide a general guideline for selecting a particular disinfectant for use with a given agent.
The best way of ascertaining the suitability of a disinfectant against a particular agent is to challenge that agent with the disinfectant at the manufacturer’s recommended concentration. A brief description of the mode of action of each class of chemical disinfectant is given below.
Although physical methods are often superior to chemical disinfection / sterilization, it is not practical to autoclave or subject many items to high heat, especially if the items can be damaged through repeated exposure to heat. Treatment of inert surfaces and heat labile materials can be accomplished through the use of disinfectants, provided that the following factors are considered:
The interplay of these factors will determine the degree of success in accomplishing either disinfection or sterilization. In all situations, review the manufacturer’s recommendations for correct formulation and use. Do not attempt to use a chemical disinfectant for a purpose it was not designed for.
Most Environmental Protection Agency (EPA)-registered disinfectants have a 10-minute label claim. However, multiple investigators have demonstrated the effectiveness of these disinfectants against vegetative bacteria (e.g., Listeria, Escherichia coli, Salmonella, vancomycin-resistant Enterococci, methicillin-resistant Staphylococcus aureus), yeasts (e.g., Candida), mycobacteria (e.g., Mycobacterium tuberculosis), and viruses (e.g. poliovirus) at exposure times of 30–60 seconds. Federal law requires all applicable label instructions on EPA-registered products to be followed (e.g., use-dilution, shelf life, storage, material compatibility, safe use, and disposal).
EPA additional resources:
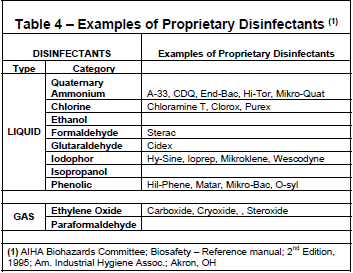
Chemical Disinfectant Groups
Aldehydes: (Formaldehyde, Paraformaldehyde, Glutaraldehyde)
Formaldehyde
Formaldehyde and its polymerized solid paraformaldehyde have broad-spectrum biocidal activity and are both effective for surface and space decontamination. As a liquid (5% concentration), formaldehyde is an effective liquid decontaminant. Its biocidal action is through alkylation of carboxyl, hydroxyl and sulfhydryl groups on proteins and the ring nitrogen atoms of purine bases. Formaldehyde’s drawbacks are reduction in efficacy at refrigeration temperature, its pungent, irritating odor, and several safety concerns. Formaldehyde is presently considered to be a carcinogen or a cancer-suspect agent according to several regulatory agencies. The OSHA 8-hour time-weighted exposure limit is 0.75 ppm.
Paraformaldehyde
A solid polymer of formaldehyde. Paraformaldehyde generates formaldehyde gas when it is depolymerized by heating to 232 to 246°C (450 to 475°F); the depolymerized material reacts with the moisture in the air to form formaldehyde gas. This process is used for the decontamination of large spaced and laminar-flow biological safety cabinets when maintenance work or filter changes require access to the sealed portion of the cabinet. A neutralization step, heating ammonium carbonate, is required prior to ventilation of the space. Formaldehyde gas can react violently or explosively (7.0 – 73% v/v in air), when exposed to incompatibles, therefore, only individuals that have specific training and have been approved by the Dept. of Environmental Health & Safety are permitted to use this gas.
Glutaraldehyde
A colorless liquid and has the sharp, pungent odor typical of all aldehydes, with an odor threshold of 0.04 parts per million (ppm). It is capable of sterilizing equipment, though to effect sterilization often requires many hours of exposure. Two percent solutions of glutaraldehyde exhibit very good activity against vegetative bacteria, spores and viruses. It is ten times more effective than formaldehyde and less toxic. However, it must be limited and controlled because of its toxic properties and hazards. It is important to avoid skin contact with glutaraldehyde as it has been documented to cause skin sensitization. Glutaraldehyde is also an inhalation hazard. The NIOSH ceiling threshold limit value is 0.2 ppm.
Cidex, a commercially prepared glutaraldehyde disinfectant is used routinely for cold surface sterilization of clinical instruments. Glutaraldehyde disinfectants should always be used in accordance with the manufacturer’s directions.
Halogen-Based Biocides: (Chlorine Compounds & Iodophores)
Chlorine Compounds
Chlorine compounds are good disinfectants on clean surfaces, but are quickly inactivated by organic matter and thus reducing the biocidal activity. They have a broad spectrum of antimicrobial activity and are inexpensive and fast acting. Hypochlorites, the most widely used of the chlorine disinfectants, are available in liquid (e.g., Sodium hypochlorite), household bleach and solid (e.g., calcium hypochlorite, sodium dichloroisocyanurate) forms. Household bleach has an available chlorine content of 5.25%, or 52,500 ppm. Because of its oxidizing power, it loses potency quickly and should be made fresh and used within the same day it is prepared. The free available chlorine levels of hypochlorite solutions in both opened and closed polyethylene containers are reduced to 40% to 50% of the original concentration over a period of one month at room temperature.
There are two potential occupational exposure hazards when using hypochlorite solutions. The first is the production of the carcinogen bis-chloromethyl ether when hypochlorite solutions come in contact with formaldehyde. The second is the rapid production of chlorine gas when hypochlorite solutions are mixed with an acid. Care must also be exercised in using chlorine – based disinfectants which can corrode or damage metal, rubber, and other susceptible surfaces. Bleached articles should never be autoclaved without reducing the bleach with sodium thiosulfate or sodium bisulfate.
Chloramine T which is prepared from sodium hypochlorite and p-toluenesulfonamide is a more stable, odorless, less corrosive form of chlorine but has decreased biocidal activity in comparison to bleach.
Iodophors
Iodophors are used both as antiseptics and disinfectants. An iodophor is a combination of iodine and a solubilizing agent or carrier; the resulting complex provides a sustained-release reservoir of iodine and releases small amounts of free iodine in aqueous solution. Antiseptic iodophors are not suitable for use as hard-surface disinfectants because they contain significantly less free iodine than do those formulated as disinfectants.
Wescodyne, Betadyne, Povidone-Iodine and other iodophors are commercially available Iodine-based disinfectants, which give good control when the manufacturer’s instructions for formulation and application are followed. Both bleach and iodophors should be made up in cold water in order to prevent breakdown of the disinfectant.
Quaternary Ammonium Compounds: (Zephirin, CDQ, A-3)
Quaternary ammonium compounds are generally odorless, colorless, nonirritating, and deodorizing. They also have some detergent action, and they are good disinfectants. However, some quaternary ammonium compounds activity is reduced in the presence of some soaps or soap residues, detergents, acids and heavy organic matter loads. They are generally ineffective against viruses, spores and Mycobacterium tuberculosis. Basically these compounds are not suitable for any type of terminal disinfection.
The mode of action of these compounds is through inactivation of energy producing enzymes, denaturation of essential cell proteins, and disruption of the cell membrane. Many of these compounds are better used in water baths, incubators, and other applications where halide or phenolic residues are not desired.
Phenolics: (O-phenophenoate-base Compounds)
Phenolics are phenol (carbolic acid) derivatives. These biocides act through membrane damage and are effective against enveloped viruses, rickettsiae, fungi and vegetative bacteria. They also retain more activity in the presence of organic material than other disinfectants. Cresols, hexachlorophene, alkyl- and chloro derivatives and diphenyls are more active than phenol itself. Available commercial products are Lysol, Pine-Sol, Amphyl, O-syl, Tergisyl, Vesphene, L- Phase and Expose.
Acids/Alkalis
Strong mineral acids and alkalis have disinfectant properties proportional to the extent of their dissociation in solution. Some hydroxides are more effective than would be predicted from their values. In general acids are better disinfectants than alkalis. Mode of action is attributed to an increase of H+ and OH– species in solutions which interfere with certain microbial functions, however the total effect is not only dependent on pH alone. Weak organic acids are more potent than inorganic acids despite low dissociation rates in solution. Action is attributed to the disruption of 2° and 3° conformation of enzymes and structural proteins.
Heavy Metals
Soluble salts of mercury, silver lactate, mercuric chloride and mercurous chloride are efficient bactericidal agents. Silver nitrate and mercuric chloride are commonly used as 1:1000 aqueous solutions. Action is through attack on protein sulfhydryl groups and disruption of enzyme functions. Organic matter can reverse the disinfectant properties of mercurials.
Caution: Please consult with EH&S’s Hazardous Materials group prior to using heavy metals because many of these must be disposed of as a hazardous waste. Specifically, disposal of elemental mercury and salts of mercury are very costly.
Alcohols
Alcohols work through the disruption of cellular membranes, solubilization of lipids, and denaturation of proteins by acting directly on S-H functional groups. Ethyl and isopropyl alcohols are the two most widely used alcohols for their biocidal activity. These alcohols are effective against lipid-containing viruses and a broad spectrum of bacterial species, but ineffective against spore-forming bacteria. They evaporate rapidly, which makes extended contact times difficult to achieve unless the items are immersed.
The optimum bactericidal concentration for ethanol and isopropanol is in the range of 60% to 90% by volume. Their cidal activity drops sharply when diluted below 50% concentration. Absolute alcohol is also not very effective. They are used to clean instruments and wipe down interior of Biological Safety Cabinets and bottles, etc. to be put into Biological Safety Cabinets. Alcohols are generally regarded as being non-corrosive.
Sterilization
Steam Autoclave
Always consult with the Autoclave Manufacturer and/or Operators Manual for proper temperature, pressure, and time because these may be different that what is specified in this document.
Only autoclaves that have been registered with EH&S may be used for the disinfection of pathogenic or “suspect” infectious materials. Each of these autoclaves has a white “EH&S” sticker on it with an assigned number. You must contact EH&S if you want to use an autoclave that has not previously been registered, assigned a number, and has not had a spore test performed within 90 days and maintenance service performed within 6 months.
The CU Biological Laboratory Waste Management Disposal Policy & Procedure requires that if an autoclave is used for the sterilization of pathogenic cultures or “suspect” infectious materials, then a commercially available Bacillus stearothermophilus or Bacillus subtilis var. niger test strips must be used at least once every 90 days to validate and document the killing efficiency of the autoclave. One copy of the test results must be posted on or near the autoclave and another copy sent to EH&S. In addition, this autoclave must be checked by an authorized service provider at least every 6 months (preferably every 60-90 days) to assure proper function, i.e., preventative maintenance, temperature calibration, and verification of adequate disinfection (if Lab does not perform Bacillus test). One copy of the current preventive maintenance record must be posted on or near the autoclave and another copy sent to EH&S.
EH&S must be notified if any EH&S registered autoclave has been removed from service, or does not pass either the spore test or maintenance service. A sign must be posted on the autoclave to note “Autoclave Out Of Service”. Do not resume using autoclave until it has been successfully repaired to meet all manufacturers’ requirements for effective disinfection. Please inform EH&S when there are changes in the autoclaves and/or their uses.
Autoclaving at a temperature of 121oC (250○F), at 15 to 20 psi is one of the most convenient and effective means of sterilization available. The time is measured after the temperature of the material being sterilized reaches 121ºC (250ºF). Care must be taken to ensure that the steam can circulate around articles in order to provide even heat distribution. The success of the sterilization is very time-dependent in liquid media, with large volumes requiring longer periods of time to reach the effective temperature within the media itself. Additionally, there should be no void spaces in the load that could insulate against the steam – this condition could prevent the transference of heat to the vessels resulting in no sterilization of the contents.
In dry loads small amounts of water should be included inside the autoclave bag to ensure sufficient moisture content within the load to allow for heat transference and distribution. Autoclave tape can be used for routine runs where glassware or sterile media are prepared before use.
Chemical Indicators
Chemical Color Change Indicators
Chemical indicators for steam autoclaving change colors after being exposed for a few minutes to normal autoclave operating temperatures of 121ºC (250ºF). Hence, chemical indicators can give a quick visual reference for heat penetration inside the autoclave. Chemical indicators should be positioned near the center of each load, and toward the bottom front of the autoclave.
Caution: Most chemical indicators can only be used to verify that your autoclave has reached normal operating temperatures for decontamination; they have no time factor. Chemical indicators alone are not designed to prove that organisms are actually killed during a decontamination cycle.
Tape Indicators
Tape indicators are adhesive backed paper tape with heat sensitive, chemical indicator markings. Commonly used heat sensitive markings include diagonal stripes (autoclave tape), and/or the word “sterile”. These markings only appear when the tape has been exposed for a few minutes to normal autoclave decontamination temperatures.
Caution: Tape indicators can only be used to verify that your autoclave has reached normal operating temperatures for decontamination; they have no time factor. Tape indicators alone are not designed to verify that organisms are actually killed during a decontamination cycle.
Biological Indicators
Biological indicators are designed to demonstrate that an autoclave is capable of killing microorganisms. EH&S recommends the use of commercially available Bacillus stearothermophilus spores to monitor the effectiveness of steam autoclaves. Follow the manufacturer’s instructions for the spore test. This test must be performed at least every 90 days. Always post the results of the test on or near the autoclave – Date Performed; Test Result; Name of Person doing test.
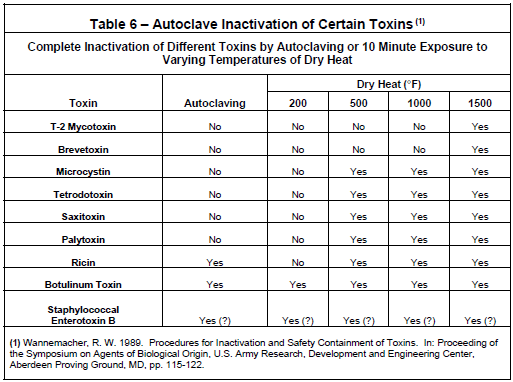
Dry Heat
Ovens operating at 160° – 170°C for periods of 2-4 hours are efficient for sterilizing glassware, or other non-porous heat conductive materials. It is unsatisfactory for organic and inorganic materials that can act as insulation and is also unsuitable for heat labile materials. Incineration is a very effective means of final sterilization and disposal, and is also used for “spot” sterilization of inoculating needles and loops as well as flaming glassware during microbiological culturing procedures. Care has to be exercised when flaming “charged” items, since this practice can release infectious micro-aerosols through spattering.
Radiation
Ionizing radiation is not used for general laboratory sterilization, however ultraviolet radiation (U.V.) is used to control airborne microorganisms and environmental surface decontamination. Ultraviolet sources are used in biological safety cabinets for partial contamination control and should be turned on only when cabinets or enclosures are not in use. This form of control is extremely limited due to its poor penetrating power, susceptibility to air movement, requirement for long contact time periods, and has not been documented as an effective control method.
The eyes and skin should not be exposed to direct or strongly reflecting UV radiation. Adequate eye and skin protection must be worn when working in an UV-irradiated area. Special safety glasses with side shields or goggles with solid side pieces should be worn. Skin protection is afforded by face shields, caps, gloves, gowns, etc.
Vapors & Gases
From a practical point of view, formaldehyde, beta-propiolactone and ethylene oxide are not routinely used in laboratory sterilization practices. These sterilants are used in hospitals and commercial facilities where closed systems controlling temperature, humidity, and concentration are required to achieve sterilization using these agents.
Of the sterilants listed above, Ethylene Oxide (ETO) has wide use as an alkyl acting agent with very broad biocide activity including spores and viruses. It is believed that the oxide ring reacts with free amino, sulfhydryl and hydroxyl groups on proteins. ETO is highly flammable and needs an inerting agent when used in a sterilizer. It is also toxic, mutagenic, and a suspected carcinogen. Additionally, beta propiolactone behaves similarly to ETO.
Useful Dilutions of Wescodyne & Common Household Bleach
Standard Wescodyne Solution
3 ounces = 90 cc; 1.2 cc / 5 gallons = 1 ppm solution
Bleach Solutions
Inactivation of Creutzfeldt-Jacobs Disease (CJD) Agent
Transmissible spongiform encephalopathies (TSEs), also known as prion diseases, are fatal degenerative brain diseases that occur in humans and certain animal species. They are characterized by microscopic vacuoles and the deposition of amyloid (prion) protein in the grey matter of the brain. All forms of TSE are experimentally transmissible.
Human TSEs occur in sporadic, familial, and acquired forms. The most common form, sporadic Creutzfeldt-Jakob disease (CJD), has a worldwide death rate of about 1 case per million people each year, and typically affects people between 55 and 75 years of age. The only infectious agent that requires unique decontamination recommendations is the prion CJD and its new variants or subpopulation of prions, vCJD’s. Infectivity is tissue dependent with the brain, spinal cord, and eye suspected to have the highest infectivity. These prions exhibit an unusual resistance to conventional chemical and physical decontamination methods. They are not adequately inactivated by most common disinfectants, or by most tissue fixatives, and some infectivity may persist under standard autoclaving conditions (e.g. 121°C for 15 minutes). They are also extremely resistant to high doses of ionizing and ultra-violet irradiation and some residual activity has been shown to survive for long periods in the environment.
The following methods have been found to be effective for the inactivation of CJD and vCJD prions:
- Steam sterilization for at least 30 minutes at a temperature of 132°C in a gravity displacement sterilizer has been recommended as the preferred method for the treatment of contaminated material.
- A prevacum sterilizer used for 18 minutes at a temperature of 134°C to 138°C has been found to be effective.
- Contaminated items such as scalpels, needles, surgical instruments, etc., immersion in 1N sodium hydroxide for 1 hour at room temperature followed by steam sterilization at 121°C for 30 minutes has been found to be effective.
- Contaminated surfaces (tabletops, floors), may be disinfected with either bleach (undiluted, or up to 1:10 dilution) or 1N sodium hydroxide at room temperature for 15 minutes or less.
- Contaminated skin surfaces are washed with 1.0N NaOH or 10% bleach for 2-3 minutes, followed by rinsing with copious amounts of water. Splashes to the eye or mouth are rinsed with copious amounts of water or saline. In both instances, inform PI or lab manager of the incident, consult with a healthcare provider (i.e. Wardenburg, WorkWell or Arbor Workman Compensation clinics depending on University employment status), and complete a University Incident Report form and returned to Risk Management. (BROKEN LINK)
References
- Manufacturing Chemists Association: Laboratory Waste Disposal Manual. Revised August 1975 MCA 1825 Connecticut Avenue, Washington DC 20009
- U.S. DHEW/P.H.S/NIH/NCI; Effective use of the Laminar Flow Biological Safety Cabinet; NCI, Bethesda, MD
- APIC (Association for Professionals in Infection Control and Epidemiology) “Guidelines for Selection and Use of Disinfectants” reprint from American Journal of Infection Control; Vol. 24, No. 4, pp. 313-342, August 1996.
- Davis, B.D. Dulbecco, R., Eisen, H.N. et al ; Microbiology, Third Edition (1980); Harper and Row; Hagerstown, MD
- Joklik W.K., Willet, H.P.; Zinsser Microbiology; 18th Edition 1984; Appleton Century- Crofts/ New York
- Block, S.S.; Disinfection, Sterilization and Preservation; 5th Edition (2000) Lippincott Williams & Wilkins; Philadelphia
- Pelczar, M.J. Reid, R.D., Chan, E.C.S.; Microbiology, 4th Edition (1977); McGraw Hill Book Company, New York
- Kruse, R.H.; Puckett, William H.; “Biological Safety Cabinetry”; Clinical Microbiological Reviews; Vol 4 (2), pp 207-241; (1991) American Society for Microbiology, Washington, D.C.
- WHO Infection Control Guidelines for Transmissible Spongiform Encephalopathies, Geneva, Switzerland, 23-26 March 1999.
